Type 2 diabetes pathophysiology is the study of the mechanisms by which type 2 diabetes develops and progresses. Type 2 diabetes is a chronic condition characterized by high blood sugar levels due to the body’s inability to effectively use insulin, a hormone that helps glucose enter cells for energy. Over time, high blood sugar levels can damage blood vessels and organs, leading to severe complications such as heart disease, stroke, kidney failure, and blindness.
Understanding the pathophysiology of type 2 diabetes is essential for developing effective treatments and prevention strategies. Research in this area has identified several key factors that contribute to the development and progression of the disease, including:
- Insulin resistance: In type 2 diabetes, the body’s cells become resistant to the effects of insulin, making it difficult for glucose to enter cells and be used for energy.
- Impaired insulin secretion: The pancreas, which produces insulin, may not be able to secrete enough insulin to overcome insulin resistance.
- Increased glucose production: The liver may produce too much glucose, further contributing to high blood sugar levels.
By understanding the pathophysiology of type 2 diabetes, researchers and healthcare professionals can develop more targeted and effective strategies for managing the condition and preventing its complications.
Type 2 Diabetes Pathophysiology
Type 2 diabetes pathophysiology encompasses various interconnected aspects that contribute to the development and progression of the disease. Understanding these key aspects is crucial for developing effective management and prevention strategies.
- Insulin Resistance: Cells become less responsive to insulin, leading to impaired glucose uptake.
- Impaired Insulin Secretion: The pancreas fails to produce sufficient insulin to overcome insulin resistance.
- Increased Glucose Production: The liver produces excessive glucose, further elevating blood sugar levels.
- Genetic Predisposition: Certain genetic variations increase the risk of developing type 2 diabetes.
- Environmental Factors: Obesity, physical inactivity, and unhealthy diet contribute to insulin resistance and impaired glucose metabolism.
- Inflammation: Chronic inflammation plays a role in the development of insulin resistance and type 2 diabetes.
These aspects are interconnected and can influence each other. For example, obesity and physical inactivity can promote inflammation, which in turn can contribute to insulin resistance. Understanding these complex interactions is essential for developing comprehensive approaches to prevent and manage type 2 diabetes.
Insulin Resistance
Insulin resistance is a hallmark of type 2 diabetes pathophysiology. In this condition, cells become less responsive to insulin, a hormone that helps glucose enter cells for energy. As a result, glucose accumulates in the bloodstream, leading to high blood sugar levels.
- Reduced Insulin Receptor Expression: Insulin resistance can occur when cells have fewer insulin receptors on their surface. This reduces the number of sites where insulin can bind and initiate its signaling cascade.
- Impaired Insulin Receptor Function: Even if cells have a normal number of insulin receptors, these receptors may not function properly in insulin-resistant individuals. This can result from defects in the insulin receptor itself or in the downstream signaling pathway.
- Increased Production of Counter-Regulatory Hormones: Insulin resistance can also be caused by increased production of counter-regulatory hormones, such as glucagon and cortisol. These hormones oppose the effects of insulin and can lead to increased glucose production and decreased glucose uptake.
- Chronic Inflammation: Chronic inflammation is another factor that can contribute to insulin resistance. Inflammatory cytokines can interfere with insulin signaling and promote the development of insulin resistance.
Insulin resistance is a complex condition that can result from a combination of genetic, environmental, and lifestyle factors. Understanding the mechanisms of insulin resistance is essential for developing effective strategies to prevent and treat type 2 diabetes.
Impaired Insulin Secretion
Impaired insulin secretion is a key factor in the pathophysiology of type 2 diabetes. In this condition, the pancreas fails to produce enough insulin to overcome insulin resistance, leading to high blood sugar levels.
- Reduced Beta-Cell Function: Beta cells in the pancreas are responsible for producing insulin. In type 2 diabetes, beta cells may not function properly, leading to reduced insulin secretion.
- Increased Beta-Cell Death: In some cases, beta cells may die prematurely, further reducing insulin production.
- Impaired Insulin Release: Even if beta cells are functioning properly, insulin may not be released into the bloodstream in a timely or sufficient manner.
- Increased Demand for Insulin: In the setting of insulin resistance, the pancreas may be unable to keep up with the increased demand for insulin, leading to impaired insulin secretion.
Impaired insulin secretion is a serious condition that can lead to severe complications. Understanding the mechanisms of impaired insulin secretion is essential for developing effective treatments for type 2 diabetes.
Increased Glucose Production
Increased glucose production by the liver, known as hepatic overproduction, is a key factor in the pathophysiology of type 2 diabetes. In this condition, the liver produces more glucose than the body needs, leading to high blood sugar levels.
- Gluconeogenesis: Gluconeogenesis is the process by which the liver produces glucose from non-carbohydrate sources, such as amino acids and fats. In type 2 diabetes, gluconeogenesis is often increased, leading to excessive glucose production.
- Glycogenolysis: Glycogenolysis is the process by which the liver breaks down stored glycogen into glucose. In type 2 diabetes, glycogenolysis may be increased, contributing to elevated blood sugar levels.
- Reduced Insulin Suppression: Insulin normally suppresses glucose production by the liver. In type 2 diabetes, insulin resistance can lead to reduced suppression of hepatic glucose production.
- Increased Counter-Regulatory Hormones: Counter-regulatory hormones, such as glucagon and cortisol, can stimulate glucose production by the liver. In type 2 diabetes, increased levels of these hormones can contribute to hepatic overproduction of glucose.
Increased glucose production by the liver is a serious condition that can lead to severe complications. Understanding the mechanisms of hepatic glucose overproduction is essential for developing effective treatments for type 2 diabetes.
Genetic Predisposition
Genetic predisposition plays a significant role in the pathophysiology of type 2 diabetes. Certain genetic variations can increase an individual’s susceptibility to developing the condition, influencing various aspects of glucose metabolism and insulin function.
- Impaired Insulin Secretion: Genetic variations in genes involved in insulin secretion, such as those encoding for the insulin gene itself or for transcription factors that regulate insulin expression, can lead to impaired insulin production and contribute to the development of type 2 diabetes.
- Insulin Resistance: Genetic variants in genes involved in insulin signaling and glucose transport can lead to insulin resistance, a key factor in the pathophysiology of type 2 diabetes. These variations may affect the expression or function of insulin receptors, downstream signaling molecules, or glucose transporters.
- Increased Glucose Production: Genetic variations in genes involved in hepatic glucose production can lead to increased glucose output by the liver, contributing to elevated blood sugar levels and the development of type 2 diabetes.
- Other Metabolic Pathways: Genetic variations in genes involved in other metabolic pathways, such as those regulating lipid metabolism or inflammation, can also influence the risk of developing type 2 diabetes by affecting insulin sensitivity, glucose homeostasis, and overall metabolic health.
Understanding the genetic basis of type 2 diabetes pathophysiology is crucial for developing personalized approaches to prevention and treatment. By identifying individuals at high genetic risk, targeted interventions can be implemented to reduce their risk of developing the disease or to delay its onset and progression.
Environmental Factors
Environmental factors significantly influence the development of type 2 diabetes pathophysiology. Obesity, physical inactivity, and unhealthy diet are key modifiable environmental factors that contribute to insulin resistance and impaired glucose metabolism, increasing the risk of developing type 2 diabetes.
- Obesity: Obesity, characterized by excessive body fat, is strongly linked to insulin resistance. Adipose tissue releases hormones and inflammatory factors that can interfere with insulin signaling and promote insulin resistance in other tissues, such as muscle and liver.
- Physical inactivity: Regular physical activity improves insulin sensitivity and glucose metabolism. Conversely, physical inactivity leads to decreased insulin sensitivity and impaired glucose uptake by muscles, contributing to the development of insulin resistance and type 2 diabetes.
- Unhealthy diet: A diet high in processed foods, sugary drinks, and saturated fats can contribute to insulin resistance and impaired glucose metabolism. These foods can lead to weight gain, inflammation, and oxidative stress, all of which can negatively impact insulin signaling and glucose homeostasis.
Understanding the role of environmental factors in type 2 diabetes pathophysiology is crucial for developing effective prevention and management strategies. By promoting healthy lifestyles that include a balanced diet, regular physical activity, and maintaining a healthy weight, individuals can reduce their risk of developing insulin resistance, impaired glucose metabolism, and ultimately type 2 diabetes.
Inflammation
Chronic inflammation is a key player in the pathophysiology of type 2 diabetes. It disrupts normal glucose metabolism and insulin signaling, contributing to insulin resistance and the development of the disease.
- Adipose Tissue Inflammation: Excess body fat, especially in the abdominal region, can lead to inflammation of adipose tissue. This inflammation releases pro-inflammatory cytokines that interfere with insulin signaling and promote insulin resistance in other tissues.
- Immune System Activation: In obesity and type 2 diabetes, the immune system becomes activated, releasing inflammatory cytokines that can damage pancreatic beta cells and impair insulin secretion.
- Oxidative Stress: Chronic inflammation generates reactive oxygen species (ROS) that can damage cells and tissues. In type 2 diabetes, ROS can impair insulin signaling and contribute to insulin resistance.
- Endoplasmic Reticulum Stress: Inflammation can activate the unfolded protein response in the endoplasmic reticulum (ER), leading to ER stress. ER stress can disrupt insulin signaling and promote beta cell dysfunction.
Understanding the role of inflammation in type 2 diabetes pathophysiology is crucial for developing effective treatments. By targeting inflammation, we may be able to prevent or delay the onset of the disease and improve outcomes for individuals with type 2 diabetes.
FAQs on Type 2 Diabetes Pathophysiology
This section addresses common questions and misconceptions surrounding type 2 diabetes pathophysiology, providing concise and informative answers.
Question 1: What is the primary mechanism underlying type 2 diabetes?
Type 2 diabetes is characterized by insulin resistance, a condition in which cells become less responsive to insulin, leading to impaired glucose uptake. This resistance can result from various factors, including obesity, physical inactivity, and genetic predisposition.
Question 2: How does obesity contribute to type 2 diabetes development?
Excess body fat, particularly in the abdominal region, can lead to inflammation of adipose tissue. This inflammation releases pro-inflammatory cytokines that interfere with insulin signaling, promoting insulin resistance in other tissues.
Question 3: What is the role of the pancreas in type 2 diabetes?
The pancreas produces insulin, a hormone responsible for facilitating glucose uptake into cells. In type 2 diabetes, the pancreas may fail to produce sufficient insulin to overcome insulin resistance, leading to high blood sugar levels.
Question 4: How does inflammation contribute to type 2 diabetes pathophysiology?
Chronic inflammation can damage pancreatic beta cells, impairing insulin secretion. Additionally, inflammation can activate the unfolded protein response, leading to ER stress and further disrupting insulin signaling.
Question 5: What are the key genetic factors that increase the risk of developing type 2 diabetes?
Genetic variations in genes involved in insulin secretion, insulin signaling, and glucose transport can predispose individuals to developing type 2 diabetes. These variations can affect the expression or function of insulin receptors, downstream signaling molecules, or glucose transporters.
Question 6: How can lifestyle modifications impact type 2 diabetes pathophysiology?
Maintaining a healthy weight through a balanced diet and regular physical activity can improve insulin sensitivity and glucose metabolism. Conversely, obesity, physical inactivity, and unhealthy diets can contribute to insulin resistance and increase the risk of developing type 2 diabetes.
Summary: Understanding type 2 diabetes pathophysiology is crucial for developing effective prevention and management strategies. By addressing key factors such as insulin resistance, the role of the pancreas, inflammation, genetic predisposition, and lifestyle influences, we can gain a comprehensive understanding of the disease and work towards improving outcomes for individuals with type 2 diabetes.
Transition to the next article section: This section will explore the latest research advancements in type 2 diabetes pathophysiology and discuss emerging therapeutic approaches for the management of the disease.
Tips for Understanding Type 2 Diabetes Pathophysiology
Grasping the intricate mechanisms underlying type 2 diabetes pathophysiology is essential for healthcare professionals and individuals affected by the condition. Here are some practical tips to enhance your understanding:
Tip 1: Focus on Key Concepts
Begin by understanding fundamental concepts such as insulin resistance, impaired insulin secretion, and increased glucose production. These concepts form the cornerstone of type 2 diabetes pathophysiology.
Tip 2: Explore Genetic and Environmental Influences
Recognize the interplay between genetic predisposition and environmental factors in the development of type 2 diabetes. Obesity, physical inactivity, and unhealthy diets are significant modifiable risk factors.
Tip 3: Study the Role of Inflammation
Comprehend the role of chronic inflammation in type 2 diabetes pathophysiology. Inflammation can damage pancreatic beta cells and impair insulin signaling, contributing to disease progression.
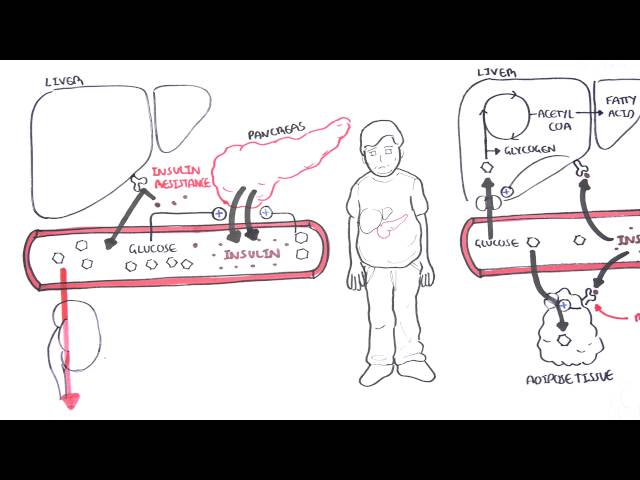
Tip 4: Utilize Visual Aids and Resources
Leverage diagrams, charts, and online resources to visualize complex concepts and pathways involved in type 2 diabetes pathophysiology. This can enhance comprehension and retention.
Tip 5: Engage in Discussions and Case Studies
Participate in discussions and analyze case studies to apply your knowledge and gain insights into real-world clinical scenarios involving type 2 diabetes pathophysiology.
Summary: By implementing these tips, you can deepen your understanding of type 2 diabetes pathophysiology, empowering yourself to make informed decisions and contribute to effective disease management.
Transition to the article’s conclusion: This comprehensive understanding lays the foundation for exploring the latest advancements and therapeutic strategies in type 2 diabetes management, as discussed in the subsequent section.
Type 2 Diabetes Pathophysiology
This exploration of type 2 diabetes pathophysiology has shed light on the complex mechanisms underlying the disease. From insulin resistance and impaired insulin secretion to increased glucose production and the role of inflammation, we have gained a comprehensive understanding of the factors that contribute to its development and progression.
This knowledge empowers us to make informed decisions regarding prevention, early detection, and effective management of type 2 diabetes. By adopting healthy lifestyles, maintaining a balanced diet, engaging in regular physical activity, and seeking timely medical advice, we can collectively work towards reducing the burden of this disease.
Youtube Video: