Injectable diabetes medications are a class of drugs used to treat diabetes. They work by mimicking the effects of insulin, a hormone produced by the pancreas that helps the body use glucose for energy.
Injectable diabetes medications are an important treatment option for people with diabetes because they can help to lower blood sugar levels and prevent complications such as heart disease, stroke, kidney disease, and blindness.
There are several different types of injectable diabetes medications, including:
- Rapid-acting insulin
- Short-acting insulin
- Intermediate-acting insulin
- Long-acting insulin
Each type of insulin has its own unique onset and duration of action, so it is important to work with a doctor to determine the best type of insulin for your individual needs.
Injectable Diabetes Medications
Injectable diabetes medications are crucial in managing diabetes, offering several key aspects that impact treatment and well-being:
- Effectiveness: Effectively lower blood sugar levels.
- Customization: Tailored to individual needs and insulin requirements.
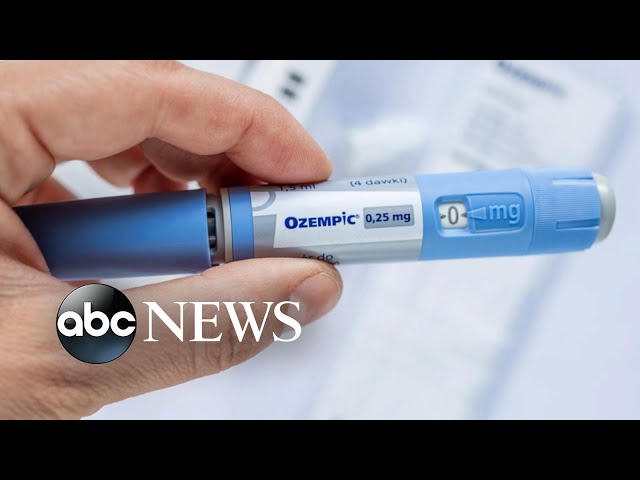
- Convenience: Pre-filled pens and vials offer ease of use.
- Rapid action: Some types provide quick correction of high blood sugar levels.
- Long-lasting effects: Extended-release formulations provide consistent blood sugar control.
- Improved outcomes: Reduce the risk of diabetes-related complications.
- Disease management: Facilitate better glucose monitoring and lifestyle adjustments.
- Patient education: Empower patients with knowledge and skills for effective self-management.
These aspects highlight the significance of injectable diabetes medications in optimizing blood sugar control, personalizing treatment, enhancing convenience, and empowering individuals to manage their diabetes effectively.
Effectiveness
Injectable diabetes medications are highly effective in lowering blood sugar levels due to their ability to mimic the effects of insulin, a hormone that facilitates glucose uptake by cells.
When blood sugar levels rise, the pancreas releases insulin to signal cells to absorb glucose for energy or storage. Injectable diabetes medications supplement or replace the body’s own insulin, allowing cells to utilize glucose effectively, thereby reducing blood sugar levels.
The effectiveness of injectable diabetes medications is crucial because elevated blood sugar levels over time can lead to severe health complications such as heart disease, stroke, kidney disease, and blindness. Effective blood sugar management is essential for preventing these complications and maintaining overall well-being.
Customization
The ability of injectable diabetes medications to be customized to individual needs and insulin requirements is of paramount importance in effective diabetes management.
Each person with diabetes has unique characteristics, such as varying degrees of insulin resistance and different activity levels. Injectable diabetes medications allow for precise tailoring of insulin doses to meet these individual needs.
For example, people with type 1 diabetes typically require multiple daily injections of a combination of rapid-acting and long-acting insulin to mimic the body’s natural insulin production. In contrast, people with type 2 diabetes may initially require only basal insulin (typically long-acting) to supplement their body’s own insulin production, with the addition of rapid-acting insulin as needed to correct high blood sugar levels.
The flexibility of injectable diabetes medications allows healthcare professionals to work closely with patients to determine the optimal insulin regimen for their individual needs, ensuring effective blood sugar control and reducing the risk of complications.
Furthermore, the availability of various insulin formulations, including pre-filled pens and vials, provides convenience and ease of use, empowering patients to manage their diabetes effectively.
Convenience
Pre-filled pens and vials have revolutionized the delivery of injectable diabetes medications, offering unparalleled convenience and ease of use for patients.
- Simplicity: Pre-filled pens eliminate the need for mixing and measuring insulin, reducing the risk of errors and simplifying the injection process.
- Discretion: Pens and vials are compact and portable, allowing for discreet injections in public or social settings, reducing the stigma associated with diabetes management.
- Accuracy: Pre-filled pens deliver precise doses of insulin, minimizing the risk of over- or under-dosing, which can lead to complications.
- Time-saving: The convenience of pre-filled pens and vials saves time compared to traditional methods of injection, making it easier for patients to fit diabetes management into their busy schedules.
The convenience offered by pre-filled pens and vials significantly improves the quality of life for people with diabetes. It empowers them to manage their condition more effectively, promotes adherence to treatment plans, and reduces the burden of diabetes on their daily lives.
Rapid action
Rapid-acting injectable diabetes medications play a crucial role in managing blood sugar levels, particularly after meals or when blood sugar levels rise unexpectedly. These medications are designed to mimic the body’s natural insulin response to food intake, allowing glucose to be quickly absorbed by cells and reducing blood sugar levels.
The rapid action of these medications is achieved through their formulation and administration. They are typically clear and colorless solutions that are injected subcutaneously (just beneath the skin) using a fine needle. This allows for rapid absorption into the bloodstream, with effects beginning within 15-30 minutes and peaking within 1-3 hours.
The ability to quickly correct high blood sugar levels is essential in preventing acute complications such as diabetic ketoacidosis (DKA) and hyperosmolar hyperglycemic syndrome (HHS). These conditions can occur when blood sugar levels become dangerously high and require immediate medical attention.
Rapid-acting injectable diabetes medications are often used in combination with other types of insulin, such as long-acting basal insulin, to provide comprehensive blood sugar control throughout the day. This combination approach helps to maintain stable blood sugar levels and reduce the risk of both high and low blood sugar episodes.
Overall, the rapid action of certain injectable diabetes medications is a critical component of effective diabetes management, allowing for quick correction of high blood sugar levels and preventing acute complications.
Long-lasting effects
Extended-release injectable diabetes medications are designed to provide consistent blood sugar control over an extended period, typically 24 hours or more. These medications are formulated to release insulin gradually into the bloodstream, mimicking the body’s natural insulin production.
- Basal insulin: Basal insulin is a long-acting insulin that provides a steady, low level of insulin throughout the day. It is typically used once or twice daily and helps to prevent blood sugar levels from rising too high between meals and overnight.
- Intermediate-acting insulin: Intermediate-acting insulin has a longer duration of action than rapid-acting insulin but a shorter duration than basal insulin. It is typically used once or twice daily and can be used to cover both basal insulin needs and post-meal blood sugar spikes.
- Premixed insulin: Premixed insulin is a combination of rapid-acting and intermediate-acting insulin in a single injection. It is typically used twice daily and can be used to cover both basal insulin needs and post-meal blood sugar spikes.
Long-lasting injectable diabetes medications are an important part of diabetes management, as they can help to keep blood sugar levels within a target range and reduce the risk of complications. They are particularly beneficial for people who have difficulty controlling their blood sugar levels with other types of diabetes medications.
Improved outcomes
Injectable diabetes medications play a crucial role in improving outcomes and reducing the risk of diabetes-related complications by effectively managing blood sugar levels.
High blood sugar levels over time can damage various organs and tissues, leading to severe complications such as:
- Heart disease
- Stroke
- Kidney disease
- Blindness
- Neuropathy (nerve damage)
- Amputations
Injectable diabetes medications help to prevent these complications by maintaining blood sugar levels within a healthy range. By doing so, they reduce the risk of damage to the blood vessels, nerves, and organs.
Studies have consistently shown that people with diabetes who use injectable diabetes medications have better blood sugar control and a lower risk of complications compared to those who do not use these medications.
For example, the ACCORD (Action to Control Cardiovascular Risk in Diabetes) trial found that people with type 2 diabetes who used injectable insulin had a 35% lower risk of cardiovascular events (such as heart attack and stroke) compared to those who used oral diabetes medications.
Another study, the ADVANCE (Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified Release Controlled Evaluation) trial, found that people with type 2 diabetes who used injectable insulin had a 21% lower risk of dying from any cause compared to those who used oral diabetes medications.
These studies and others provide strong evidence that injectable diabetes medications are effective in reducing the risk of diabetes-related complications and improving outcomes for people with diabetes.
Disease management
Injectable diabetes medications play a crucial role in facilitating better glucose monitoring and lifestyle adjustments, which are essential components of effective disease management for people with diabetes.
Glucose monitoring involves regularly checking blood sugar levels to understand how they respond to different foods, activities, and medications. Accurate glucose monitoring is crucial for making informed decisions about insulin doses and lifestyle choices.
Injectable diabetes medications provide a precise and convenient way to control blood sugar levels. By using these medications, people with diabetes can better manage their glucose levels and reduce the risk of developing complications.
Additionally, injectable diabetes medications can help people with diabetes make healthier lifestyle adjustments. For example, by stabilizing blood sugar levels, these medications can improve energy levels and reduce fatigue, making it easier to engage in regular physical activity.
Furthermore, injectable diabetes medications can help reduce cravings and improve overall well-being, making it easier to adopt and maintain a healthy diet.
Overall, injectable diabetes medications are essential tools for disease management in people with diabetes. They facilitate better glucose monitoring and lifestyle adjustments, which are crucial for preventing complications and improving quality of life.
Patient education
Patient education is a crucial aspect of injectable diabetes medications, empowering individuals with the knowledge and skills necessary for effective self-management.
- Understanding Injectable Diabetes Medications: Patients learn about the different types of injectable diabetes medications, their mechanisms of action, and how to use and store them properly. This knowledge enables them to make informed decisions about their treatment plan and avoid potential complications.
- Glucose Monitoring: Education on glucose monitoring techniques, including how to use a glucometer and interpret blood sugar readings, is essential. Patients can track their blood sugar levels and adjust their insulin doses accordingly, promoting better control.
- Insulin Administration Techniques: Patients receive training on proper injection techniques, including choosing the right injection site, rotating injection sites, and handling syringes or pens safely. This knowledge ensures accurate and effective insulin delivery.
- Lifestyle Management: Education extends beyond medication management to encompass lifestyle modifications, such as healthy eating habits, regular exercise, and stress management. Patients learn how these factors impact blood sugar levels and how to make sustainable changes for improved overall health.
Empowering patients with thorough education enables them to become active participants in their diabetes management. They gain confidence in managing their condition, reducing the burden of diabetes and improving their quality of life.
FAQs on Injectable Diabetes Medications
Injectable diabetes medications are a cornerstone of diabetes management, offering effective blood sugar control and reducing the risk of complications. Here are answers to some frequently asked questions:
Question 1: What are the different types of injectable diabetes medications?
There are several types of injectable diabetes medications, including rapid-acting, short-acting, intermediate-acting, and long-acting insulin. Each type has its unique onset and duration of action, allowing for customized treatment plans.
Question 2: How are injectable diabetes medications administered?
Injectable diabetes medications are typically administered subcutaneously, meaning they are injected just beneath the skin. They can be injected using syringes, pens, or insulin pumps.
Question 3: What are the benefits of using injectable diabetes medications?
Injectable diabetes medications offer several benefits, including effective blood sugar control, reduced risk of complications, improved quality of life, and increased flexibility in managing diabetes.
Question 4: Are there any side effects associated with injectable diabetes medications?
Like all medications, injectable diabetes medications can have side effects, such as hypoglycemia (low blood sugar), weight gain, and injection site reactions. However, these side effects can usually be managed with proper monitoring and medical guidance.
Question 5: How can I learn more about injectable diabetes medications?
Consult your healthcare provider or a diabetes educator for detailed information and guidance on injectable diabetes medications. They can provide personalized advice based on your individual needs and circumstances.
Question 6: What is the future of injectable diabetes medications?
Research and development in injectable diabetes medications are ongoing, with a focus on improving insulin delivery systems, enhancing insulin stability, and developing new formulations for better efficacy and patient convenience.
Summary: Injectable diabetes medications are effective and essential treatment options for managing diabetes. They offer personalized blood sugar control, reduce the risk of complications, and improve overall well-being. By working closely with healthcare providers and adhering to proper medication management, individuals with diabetes can effectively manage their condition and live fulfilling lives.
Transition: The next section of this article will explore the latest advancements in diabetes technology, including continuous glucose monitoring systems and insulin pumps, which further enhance diabetes management and improve patient outcomes.
Injectable Diabetes Medications
Injectable diabetes medications are powerful tools for managing blood sugar levels and preventing complications. Here are some essential tips to optimize their use:
Tip 1: Adhere to Prescribed Regimen:
Follow your healthcare provider’s instructions carefully regarding the type, dosage, and timing of your insulin injections. Consistency is crucial for maintaining stable blood sugar levels.
Tip 2: Monitor Blood Sugar Regularly:
Regular blood sugar monitoring is essential for assessing the effectiveness of your insulin therapy. Test your blood sugar levels as directed by your healthcare provider, especially before meals, after physical activity, and before bedtime.
Tip 3: Learn Proper Injection Techniques:
Mastering proper injection techniques ensures accurate and effective insulin delivery. Ask your healthcare provider or diabetes educator to demonstrate the correct steps, including choosing the right injection site and rotating injection sites.
Tip 4: Store Insulin Correctly:
Store your insulin according to the manufacturer’s instructions to maintain its potency. Keep unopened vials refrigerated, and protect opened vials from extreme temperatures and sunlight.
Tip 5: Manage Hypoglycemia:
Hypoglycemia (low blood sugar) can occur if your insulin dose is too high. Always carry a fast-acting source of sugar, such as glucose tablets or juice, to treat hypoglycemia promptly.
Tip 6: Adjust Insulin Doses as Needed:
Your insulin needs may change over time due to factors like diet, activity level, and illness. Consult with your healthcare provider regularly to adjust your insulin doses as necessary to maintain optimal blood sugar control.
Tip 7: Attend Diabetes Education Classes:
Diabetes education classes provide valuable information on diabetes management, including proper use of injectable diabetes medications, glucose monitoring, and lifestyle modifications. These classes empower you with the knowledge and skills to manage your condition effectively.
Summary: Injectable diabetes medications are essential for managing blood sugar levels and preventing diabetes complications. By following these tips, you can optimize the effectiveness of your insulin therapy, maintain stable blood sugar levels, and improve your overall well-being.
Transition: The successful management of diabetes involves a multifaceted approach. The next section will delve into additional strategies, including lifestyle modifications and technological advancements, to enhance diabetes management and improve patient outcomes.
Injectable Diabetes Medications
Injectable diabetes medications play a pivotal role in the management of diabetes, offering effective blood sugar control and reducing the risk of associated complications. Their customizable nature, ease of use, and ability to mimic the body’s natural insulin production make them a cornerstone of diabetes treatment.
This article comprehensively explored the various aspects of injectable diabetes medications, including their types, benefits, administration techniques, and strategies for effective management. By understanding and adhering to the proper use of these medications, individuals with diabetes can optimize their blood sugar control, improve their quality of life, and prevent long-term complications.
As research and innovation continue, the future of diabetes management holds promise for even more advanced and personalized injectable diabetes medications. The ongoing development of insulin delivery systems, improved formulations, and integrated technologies will further empower individuals with diabetes to effectively manage their condition and live healthier, more fulfilling lives.
Youtube Video: