Diabetes injections are a crucial treatment method for individuals living with diabetes, a chronic condition that affects the body’s ability to regulate blood sugar levels. These injections provide the essential insulin hormone, which enables cells to absorb glucose from the bloodstream for energy.
Insulin injections have revolutionized diabetes management since their discovery, enabling people with diabetes to control their blood sugar levels effectively and manage their condition. They have significantly reduced the risk of severe complications associated with diabetes, such as diabetic ketoacidosis, heart disease, and kidney failure.
The main article will delve into the types of diabetes injections available, their administration methods, potential side effects, and the importance of adhering to prescribed injection regimens. It will also explore the latest advancements in diabetes injection technology and research.
Diabetes Injections
Diabetes injections are a vital treatment for individuals with diabetes, providing essential insulin to regulate blood sugar levels and prevent severe complications.
- Types: Basal, bolus, premixed
- Administration: Subcutaneous, intravenous
- Dosage: Determined by individual needs and blood sugar levels
- Benefits: Improved blood sugar control, reduced risk of complications
- Side Effects: Hypoglycemia, injection site reactions
- Advancements: Insulin pumps, continuous glucose monitors
- Adherence: Crucial for effective diabetes management
These key aspects collectively underscore the significance of diabetes injections in managing diabetes effectively. Adhering to prescribed injection regimens, understanding the different types and administration methods, and being aware of potential benefits and side effects are crucial for individuals with diabetes to maintain optimal health outcomes.
Types
Diabetes injections encompass three primary types: basal, bolus, and premixed. Each type plays a distinct role in regulating blood sugar levels, tailored to individual needs and lifestyle factors:
- Basal insulin: Long-acting insulin that provides a steady background level of insulin over 24 hours. It helps prevent blood sugar levels from rising too high after fasting, such as overnight or between meals.
- Bolus insulin: Rapid-acting insulin that is taken before meals to cover the rise in blood sugar caused by food. It helps bring blood sugar levels down to the target range after eating.
- Premixed insulin: Combines both basal and bolus insulin in one injection, providing a mix of long-acting and rapid-acting insulin. It offers convenience but may not be as flexible as separate basal and bolus injections.
Understanding the different types of diabetes injections is essential for effective diabetes management. Healthcare providers work with individuals to determine the most appropriate type and dosage based on their specific needs and blood sugar control goals.
Administration
Diabetes injections are typically administered subcutaneously, meaning into the fatty tissue just beneath the skin. This method is preferred due to its simplicity, relatively low risk of complications, and ability to provide sustained insulin delivery.
In certain circumstances, such as during emergencies or when rapid insulin delivery is necessary, intravenous (IV) administration may be used. IV injections deliver insulin directly into a vein, resulting in a faster onset of action. However, IV injections require a healthcare professional to administer and are typically reserved for specific medical situations.
Understanding the different administration methods for diabetes injections is important for ensuring proper insulin delivery and effective blood sugar management. Healthcare providers will provide detailed instructions on injection techniques, including the appropriate injection site, needle size, and depth of injection.
Dosage
The dosage of diabetes injections is not a one-size-fits-all approach. It is carefully determined based on individual needs and blood sugar levels to ensure optimal blood sugar control while minimizing the risk of complications.
- Tailored to Individual Needs: Each person with diabetes has unique factors that influence their insulin needs, such as age, weight, activity level, and underlying health conditions. The dosage is adjusted to meet the specific needs of the individual, ensuring effective blood sugar management.
- Blood Sugar Monitoring: Regular blood sugar monitoring is crucial in determining the appropriate dosage. Blood sugar levels provide valuable insights into how the body is responding to insulin and whether adjustments are necessary. Based on the blood sugar readings, healthcare providers can fine-tune the dosage to achieve optimal control.
- Lifestyle Considerations: Lifestyle factors, such as diet and exercise, can impact insulin needs. The dosage may need to be adjusted based on changes in food intake, physical activity levels, or other lifestyle factors that affect blood sugar control.
- Periodic Adjustments: Over time, insulin needs may change due to various factors, such as changes in weight, insulin resistance, or illness. Regular check-ups and blood sugar monitoring allow healthcare providers to assess the need for dosage adjustments to maintain effective blood sugar control.
Understanding the factors that determine the dosage of diabetes injections is essential for effective diabetes management. By considering individual needs, blood sugar levels, and lifestyle factors, healthcare providers can personalize the dosage to optimize blood sugar control and improve overall health outcomes.
Benefits
Diabetes injections have revolutionized diabetes management by providing individuals with the ability to control their blood sugar levels effectively, significantly reducing the risk of severe complications associated with diabetes.
- Improved Blood Sugar Control: Insulin injections provide the necessary insulin hormone to facilitate the absorption of glucose from the bloodstream into cells for energy. This helps maintain blood sugar levels within a healthy range, preventing both high blood sugar levels (hyperglycemia) and low blood sugar levels (hypoglycemia), which can cause a range of symptoms and long-term health problems.
-
Reduced Risk of Complications: Maintaining stable blood sugar levels through diabetes injections reduces the risk of developing severe complications, including:
- Heart disease and stroke
- Kidney disease
- Eye damage, including diabetic retinopathy and macular degeneration
- Nerve damage, leading to numbness, tingling, and pain in the hands and feet
In summary, diabetes injections are a vital tool for improving blood sugar control and reducing the risk of complications associated with diabetes. By effectively managing blood sugar levels, individuals can significantly improve their overall health and well-being.
Side Effects
Diabetes injections are an essential treatment option for managing blood sugar levels in individuals with diabetes. While these injections offer significant benefits, it is important to be aware of potential side effects, including hypoglycemia (low blood sugar) and injection site reactions.
-
Hypoglycemia
Hypoglycemia occurs when blood sugar levels drop too low, often due to too much insulin or too little food intake. Symptoms can include sweating, shaking, hunger, confusion, and in severe cases, seizures or loss of consciousness. It is crucial to manage blood sugar levels carefully and follow medical instructions to prevent hypoglycemia.
-
Injection Site Reactions
Injection site reactions are common and typically mild, causing redness, swelling, or itching at the injection site. These reactions usually resolve within a few days. However, in rare cases, more severe reactions, such as lipohypertrophy (thickening of the skin) or lipoatrophy (thinning of the skin), may occur. Proper injection techniques and rotating injection sites can help minimize these reactions.
Understanding these potential side effects and taking steps to prevent or manage them is essential for safe and effective diabetes management. Regular monitoring of blood sugar levels, proper injection techniques, and open communication with healthcare providers are key to optimizing the benefits of diabetes injections while minimizing risks.
Advancements
Advancements in diabetes management technology, including insulin pumps and continuous glucose monitors (CGMs), have revolutionized diabetes injections by enhancing blood sugar control and simplifying diabetes management.
Insulin pumps are small, computerized devices that deliver insulin continuously throughout the day. They can be programmed to provide different basal rates at different times, allowing for more precise insulin delivery than multiple daily injections. Insulin pumps also have the ability to deliver bolus doses of insulin before meals, providing greater flexibility and convenience in managing blood sugar levels after eating.
CGMs are devices that continuously measure glucose levels in the interstitial fluid, providing real-time data on blood sugar trends and patterns. This information can help individuals with diabetes make informed decisions about insulin dosing, diet, and exercise, leading to improved blood sugar control and reduced risk of complications.
The combination of insulin pumps and CGMs has significantly improved the quality of life for many people with diabetes. These advancements have enabled them to achieve better blood sugar control, reduce the frequency of hypoglycemia and hyperglycemia, and enjoy greater freedom and flexibility in their daily lives.
Adherence
Adherence to prescribed diabetes injections is paramount for effective diabetes management. Injections provide the necessary insulin to regulate blood sugar levels, and consistent adherence ensures optimal glycemic control and reduces the risk of complications.
Non-adherence to diabetes injections can lead to uncontrolled blood sugar levels, increasing the risk of both acute and long-term complications. These complications can include hypoglycemia (low blood sugar), hyperglycemia (high blood sugar), diabetic ketoacidosis, cardiovascular disease, kidney disease, and blindness. Furthermore, poor adherence can lead to insulin resistance, making it more difficult to achieve glycemic control.
Practical strategies to improve adherence include setting reminders, using pill organizers, and involving family or friends in supporting adherence. Additionally, healthcare providers should provide clear instructions on injection techniques, dosage, and potential side effects, and address any concerns or barriers to adherence.
Diabetes Injections FAQs
This section provides answers to frequently asked questions about diabetes injections, aiming to provide clear and informative guidance for effective diabetes management.
Question 1: What are the different types of diabetes injections?
Answer: There are three main types of diabetes injections: basal, bolus, and premixed. Basal insulin provides a steady background level of insulin over 24 hours, while bolus insulin is taken before meals to cover the rise in blood sugar caused by food. Premixed insulin combines both basal and bolus insulin in one injection.
Question 2: How are diabetes injections administered?
Answer: Diabetes injections are typically administered subcutaneously, meaning into the fatty tissue just beneath the skin. In certain circumstances, intravenous (IV) administration may be used for rapid insulin delivery.
Question 3: How is the dosage of diabetes injections determined?
Answer: The dosage of diabetes injections is tailored to individual needs and blood sugar levels. Factors such as age, weight, activity level, and underlying health conditions are considered to determine the appropriate dosage.
Question 4: What are the potential benefits of diabetes injections?
Answer: Diabetes injections provide essential insulin to regulate blood sugar levels, preventing both high and low blood sugar levels. This helps reduce the risk of severe complications such as heart disease, kidney disease, and eye damage.
Question 5: Are there any side effects associated with diabetes injections?
Answer: Common side effects include hypoglycemia (low blood sugar) and injection site reactions. More severe reactions are rare but can include lipohypertrophy (thickening of the skin) or lipoatrophy (thinning of the skin).
Question 6: How can I improve adherence to my diabetes injection regimen?
Answer: Adherence is crucial for effective diabetes management. Setting reminders, using pill organizers, and involving family or friends can support adherence. Healthcare providers can also provide clear instructions and address any concerns or barriers.
Summary: Diabetes injections are a vital tool for managing blood sugar levels and reducing the risk of complications. Understanding the different types, administration methods, dosage determination, benefits, side effects, and strategies to improve adherence is essential for effective diabetes management.
Transition to the next article section: For further information on diabetes injections, including advanced technologies and lifestyle considerations, please refer to the following sections.
Tips for Effective Diabetes Injections
Diabetes injections play a crucial role in managing blood sugar levels and preventing complications. Here are essential tips for optimizing the effectiveness and safety of your injections:
Tip 1: Proper Injection Technique
- Use a new needle for each injection, and dispose of it safely afterward.
- Inject into clean, dry skin, and rotate injection sites to prevent lipohypertrophy or lipoatrophy.
- Pinch the skin at the injection site to create a small fold, and inject the needle perpendicularly into the fatty tissue.
Tip 2: Accurate Dosage and Timing
- Follow your healthcare provider’s instructions precisely regarding the type, dosage, and timing of your injections.
- Monitor your blood sugar levels regularly, and adjust your dosage as needed based on your healthcare provider’s guidance.
- Never skip or delay your injections, as consistent use is essential for effective blood sugar control.
Tip 3: Safe Storage and Handling
- Store insulin in the refrigerator, and allow it to warm to room temperature before injection.
- Never freeze insulin or expose it to extreme heat, as this can affect its potency.
- Discard any insulin that is cloudy, discolored, or past its expiration date.
Tip 4: Monitor for Side Effects
- Be aware of potential side effects of diabetes injections, such as hypoglycemia, injection site reactions, and lipohypertrophy.
- Report any unusual symptoms or concerns to your healthcare provider promptly.
- Carry a source of fast-acting sugar, such as glucose tablets or candy, in case of hypoglycemia.
Tip 5: Healthy Lifestyle Habits
- Maintain a healthy diet, engage in regular physical activity, and get enough sleep to support your overall diabetes management.
- Smoking and excessive alcohol consumption can interfere with blood sugar control and increase the risk of complications.
- Regular check-ups with your healthcare provider are essential for monitoring your progress and adjusting your treatment plan as needed.
By following these tips, you can optimize the effectiveness and safety of your diabetes injections, leading to better blood sugar control and improved overall health outcomes.
Conclusion: Diabetes injections are a vital part of managing diabetes and preventing complications. By understanding and implementing these tips, individuals with diabetes can effectively manage their blood sugar levels and live healthier, more fulfilling lives.
Conclusion
Diabetes injections have revolutionized the management of diabetes, enabling individuals to effectively regulate their blood sugar levels and prevent severe complications. Through advancements in insulin formulations, delivery devices, and monitoring technologies, diabetes injections continue to improve the quality of life for people with diabetes.
Adherence to prescribed injection regimens remains crucial for successful diabetes management. By understanding the different types, administration methods, dosage determination, benefits, side effects, and strategies to improve adherence, individuals can optimize the effectiveness and safety of their diabetes injections.
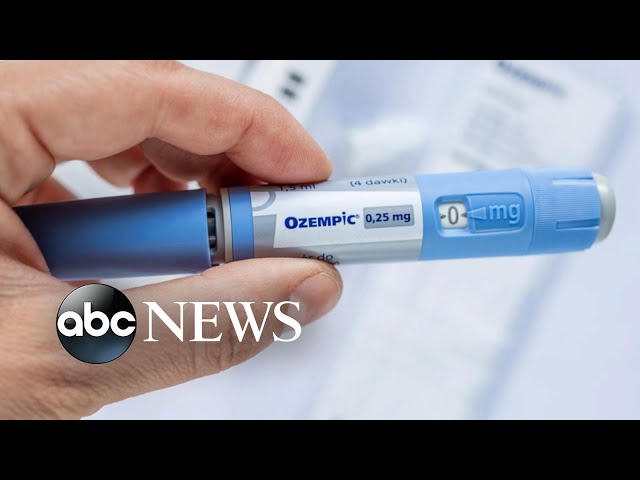
Youtube Video: