Type II Diabetes Mellitus is a chronic metabolic disorder characterized by elevated blood sugar levels due to the body’s inability to produce or effectively utilize insulin. This condition results from a combination of genetic predisposition and lifestyle factors.
Understanding Type II Diabetes Mellitus is crucial for its effective management and prevention. It is a prevalent health concern, affecting a significant portion of the population globally. Proper management can help individuals maintain a good quality of life and reduce the risk of developing severe complications such as heart disease, stroke, kidney failure, and blindness.
Various lifestyle modifications, including maintaining a healthy weight, engaging in regular physical activity, and adopting a balanced diet, play a vital role in managing Type II Diabetes Mellitus. Moreover, advancements in medical research have led to the development of effective medications that aid in regulating blood sugar levels and managing the condition.
Type II Diabetes Mellitus
Type II Diabetes Mellitus, a prevalent chronic condition, warrants attention to its essential aspects for effective management and prevention.
- Definition: Impaired insulin production or utilization, leading to elevated blood sugar levels.
- Causes: Genetic predisposition, lifestyle factors (e.g., obesity, inactivity).
- Symptoms: Frequent urination, excessive thirst, unexplained weight loss.
- Complications: Increased risk of heart disease, stroke, kidney failure, blindness.
- Diagnosis: Blood tests (e.g., fasting blood glucose, HbA1c).
- Treatment: Lifestyle changes (diet, exercise), medications (e.g., metformin, insulin).
- Prevention: Maintaining a healthy weight, regular physical activity, balanced diet.
- Management: Regular monitoring of blood sugar levels, adherence to treatment plan.
Understanding these key aspects is paramount. For instance, recognizing the dual factors of genetic predisposition and lifestyle choices in its development highlights the importance of preventive measures. The potential complications underscore the critical need for proper management to mitigate these risks. Moreover, the availability of effective treatments and the emphasis on self-management through lifestyle modifications empower individuals to take an active role in their health journey.
Definition
Within the context of Type II Diabetes Mellitus, understanding the definition of impaired insulin production or utilization leading to elevated blood sugar levels is critical. Insulin, a hormone produced by the pancreas, plays a pivotal role in regulating blood sugar levels by enabling glucose to enter cells for energy utilization. In Type II Diabetes Mellitus, the body either does not produce enough insulin or does not use insulin effectively, resulting in an inability to maintain normal blood sugar levels. This leads to a buildup of glucose in the bloodstream, characterized by persistently high blood sugar levels.
The significance of this definition lies in its direct connection to the pathophysiology of Type II Diabetes Mellitus. Impaired insulin production or utilization is the fundamental mechanism underlying the development and progression of this condition. Comprehending this definition empowers individuals to recognize the importance of maintaining healthy insulin function and, thereby promoting preventive measures and facilitating effective self-management strategies.
In practical terms, recognizing the role of impaired insulin production or utilization can guide lifestyle modifications and treatment approaches. For instance, individuals can focus on adopting a balanced diet, engaging in regular physical activity, and maintaining a healthy weight to improve insulin sensitivity and reduce the risk of developing Type II Diabetes Mellitus. Additionally, adherence to prescribed medications, such as insulin or other glucose-lowering agents, becomes crucial in managing blood sugar levels effectively.
Causes
The connection between causes, including genetic predisposition and lifestyle factors such as obesity and inactivity, and Type II Diabetes Mellitus is crucial for understanding the development and progression of this condition.
Genetic predisposition refers to the inherited susceptibility to developing Type II Diabetes Mellitus. Certain genetic variations can affect insulin production and function, increasing an individual’s risk of developing the condition. However, the presence of genetic predisposition alone does not guarantee the development of Type II Diabetes Mellitus. Lifestyle factors play a significant role in determining whether genetic predisposition translates into actual disease manifestation.
Obesity, characterized by excessive body fat, and inactivity, referring to a lack of regular physical activity, are prominent lifestyle factors that contribute to the development of Type II Diabetes Mellitus. Obesity can lead to insulin resistance, a condition where the body’s cells do not respond effectively to insulin, resulting in elevated blood sugar levels. Inactivity, on the other hand, reduces the body’s ability to utilize glucose effectively, further contributing to high blood sugar levels.
Understanding the connection between these causes and Type II Diabetes Mellitus is essential for preventive measures and effective management. Identifying individuals at risk due to genetic predisposition allows for targeted interventions and lifestyle modifications to reduce their likelihood of developing the condition. Additionally, promoting healthy lifestyle choices, such as maintaining a healthy weight and engaging in regular physical activity, becomes paramount in preventing or delaying the onset of Type II Diabetes Mellitus.
Symptoms
The connection between the symptoms of frequent urination, excessive thirst, and unexplained weight loss, and type II diabetes mellitus is crucial for understanding the condition’s progression and impact on an individual’s health.
These symptoms arise due to the body’s inability to effectively utilize glucose for energy, leading to elevated blood sugar levels. The kidneys work to filter excess glucose from the blood, resulting in frequent urination. Excessive thirst, known as polydipsia, occurs as the body attempts to replenish the fluids lost through frequent urination. Unexplained weight loss is another common symptom, as the body breaks down fat and muscle tissues for energy due to the lack of available glucose.
Recognizing these symptoms is essential for early diagnosis and intervention. They serve as indicators of the underlying metabolic disturbances in type II diabetes mellitus, prompting individuals to seek medical attention and appropriate management. Prompt diagnosis and treatment can help prevent the progression of the condition and reduce the risk of severe complications, such as heart disease, stroke, kidney failure, and blindness.
Understanding the connection between these symptoms and type II diabetes mellitus empowers individuals to take proactive steps towards managing their health. By paying attention to their bodies and recognizing these symptoms, they can initiate timely conversations with healthcare professionals, leading to appropriate screening, diagnosis, and treatment plans.
Complications
Type II Diabetes Mellitus poses significant health risks, including an increased likelihood of developing severe complications. These complications, such as heart disease, stroke, kidney failure, and blindness, arise from the body’s inability to effectively utilize glucose for energy, leading to elevated blood sugar levels.
Sustained high blood sugar levels can damage blood vessels and nerves throughout the body, increasing the risk of heart disease and stroke. The risk of heart disease is particularly high in individuals with Type II Diabetes Mellitus, as they often have other risk factors such as high blood pressure and high cholesterol.
Similarly, the kidneys work harder to filter excess glucose from the blood, which can lead to kidney damage and kidney failure. High blood sugar levels can also damage the nerves and blood vessels in the eyes, potentially leading to vision loss and blindness.
Understanding the connection between Type II Diabetes Mellitus and its potential complications is crucial for effective management. Regular monitoring of blood sugar levels, adherence to treatment plans, and lifestyle modifications, such as maintaining a healthy weight and engaging in regular physical activity, are essential in reducing the risk of developing these complications.
Early diagnosis and intervention are vital in preventing or delaying the onset of complications associated with Type II Diabetes Mellitus. Individuals with risk factors, such as a family history of diabetes or obesity, should be aware of the potential complications and take proactive steps to manage their health.
Diagnosis
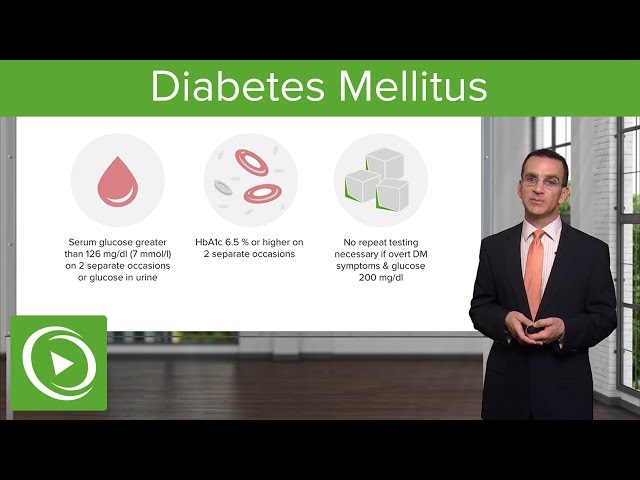
Establishing a definitive diagnosis of Type II Diabetes Mellitus relies heavily on blood tests, particularly fasting blood glucose and HbA1c tests. These tests provide crucial information about an individual’s blood sugar levels and help healthcare professionals assess the severity of the condition.
Fasting blood glucose measures the blood sugar level after a period of fasting, typically overnight. Elevated fasting blood glucose levels may indicate impaired glucose metabolism and potential diabetes. HbA1c, also known as glycated hemoglobin, reflects the average blood sugar levels over the preceding 2-3 months. It provides a comprehensive assessment of an individual’s glucose control over time.
The diagnosis of Type II Diabetes Mellitus is established when fasting blood glucose levels meet or exceed 126 mg/dL on two separate occasions or when HbA1c levels reach or surpass 6.5%. These diagnostic criteria serve as essential benchmarks for healthcare professionals to identify individuals with Type II Diabetes Mellitus and initiate appropriate treatment plans.
Understanding the connection between blood tests and the diagnosis of Type II Diabetes Mellitus is crucial for effective management and prevention. Regular monitoring of blood sugar levels through these tests allows individuals to track their progress, adjust their treatment strategies as needed, and minimize the risk of developing severe complications.
Treatment
The effective management of Type II Diabetes Mellitus involves a comprehensive approach that encompasses lifestyle modifications and pharmacological interventions. These treatments aim to improve glycemic control and minimize the risk of developing severe complications.
-
Lifestyle Changes:
Adopting a balanced diet and engaging in regular physical activity are essential pillars in the management of Type II Diabetes Mellitus. Dietary modifications focus on consuming nutrient-rich foods, such as fruits, vegetables, and whole grains, while limiting processed foods, sugary drinks, and unhealthy fats. Regular exercise enhances insulin sensitivity and improves glucose utilization, aiding in blood sugar control.
-
Medications:
In cases where lifestyle changes alone are insufficient to achieve optimal glycemic control, medications may be prescribed. Metformin is a commonly used medication that improves insulin sensitivity and reduces glucose production by the liver. Insulin therapy may also be necessary to supplement the body’s insulin production.
Understanding the connection between treatment options and Type II Diabetes Mellitus is crucial for effective self-management and improved health outcomes. Adhering to prescribed treatment plans, including lifestyle modifications and medications, empowers individuals to manage their blood sugar levels effectively and minimize the risk of complications.
Prevention
Prevention plays a crucial role in combating Type II Diabetes Mellitus, and adopting a healthy lifestyle is paramount. Maintaining a healthy weight, engaging in regular physical activity, and adhering to a balanced diet are fundamental pillars in preventing or delaying the onset of this condition.
-
Maintaining a Healthy Weight:
Excess weight, particularly around the abdomen, contributes to insulin resistance, a precursor to Type II Diabetes Mellitus. Maintaining a healthy weight through a calorie-controlled diet and regular exercise helps improve insulin sensitivity and reduces the risk of developing the condition.
-
Regular Physical Activity:
Engaging in regular physical activity enhances the body’s ability to utilize glucose effectively. Exercise increases insulin sensitivity, allowing cells to take up more glucose from the bloodstream, thereby lowering blood sugar levels.
-
Balanced Diet:
Adopting a balanced diet rich in fruits, vegetables, and whole grains provides the body with essential nutrients while limiting processed foods, sugary drinks, and unhealthy fats. A balanced diet helps regulate blood sugar levels and promotes overall well-being.
Integrating these preventive measures into one’s lifestyle is crucial for reducing the risk of Type II Diabetes Mellitus. By maintaining a healthy weight, engaging in regular physical activity, and adhering to a balanced diet, individuals can empower themselves to prevent or delay the onset of this condition and promote overall health and well-being.
Management
Effective management of Type II Diabetes Mellitus hinges on regular monitoring of blood sugar levels and strict adherence to the prescribed treatment plan. This plays a pivotal role in maintaining glycemic control, preventing complications, and promoting overall well-being.
Regular blood sugar monitoring allows individuals to track their glucose levels and make necessary adjustments to their diet, exercise, and medication regimen. By closely monitoring blood sugar levels, individuals can identify patterns, anticipate potential issues, and respond promptly to prevent extreme fluctuations.
Adherence to the treatment plan, as prescribed by healthcare professionals, is equally crucial. This may include lifestyle modifications, such as maintaining a healthy diet and engaging in regular physical activity, as well as taking prescribed medications, such as insulin or oral hypoglycemic agents. By adhering to the treatment plan, individuals can effectively manage their blood sugar levels and minimize the risk of complications.
The connection between regular monitoring of blood sugar levels and adherence to the treatment plan in Type II Diabetes Mellitus is vital for achieving optimal health outcomes. Through diligent self-management, individuals can empower themselves to manage their condition effectively, prevent complications, and live fulfilling lives.
Frequently Asked Questions about Type II Diabetes Mellitus
Individuals seeking information on Type II Diabetes Mellitus often have common concerns and misconceptions. To clarify these matters, we have compiled a list of frequently asked questions and provided informative answers to guide your understanding.
Question 1: What is the primary cause of Type II Diabetes Mellitus?
Type II Diabetes Mellitus is primarily caused by a combination of factors, including genetic predisposition and lifestyle habits. While genetic factors can increase an individual’s susceptibility, lifestyle choices, such as lack of physical activity, unhealthy diet, and obesity, play a significant role in the development of the condition.
Question 2: Can Type II Diabetes Mellitus be prevented?
While genetic predisposition cannot be altered, lifestyle modifications can significantly reduce the risk of developing Type II Diabetes Mellitus. Maintaining a healthy weight, engaging in regular physical activity, and adopting a balanced diet rich in fruits, vegetables, and whole grains are key preventive measures.
Question 3: What are the common symptoms of Type II Diabetes Mellitus?
Type II Diabetes Mellitus often develops gradually, and symptoms may be subtle initially. Common signs include increased thirst, frequent urination, unexplained weight loss, fatigue, and blurred vision. It is important to consult a healthcare professional if you experience any of these symptoms.
Question 4: How is Type II Diabetes Mellitus diagnosed?
Diagnosis of Type II Diabetes Mellitus typically involves a physical examination and blood tests. Fasting blood glucose levels and HbA1c levels are commonly used to assess blood sugar control and diagnose the condition.
Question 5: What are the potential complications of Type II Diabetes Mellitus?
Uncontrolled Type II Diabetes Mellitus can lead to various complications, including heart disease, stroke, kidney failure, nerve damage, and eye problems. Regular monitoring and adherence to treatment plans are crucial to minimize the risk of these complications.
Question 6: How is Type II Diabetes Mellitus treated?
Treatment for Type II Diabetes Mellitus involves a combination of lifestyle modifications and medications. Lifestyle changes, such as weight management, physical activity, and dietary adjustments, are essential. Medications, such as metformin, insulin, or other glucose-lowering agents, may be prescribed to manage blood sugar levels.
Understanding these frequently asked questions about Type II Diabetes Mellitus can help individuals gain a clearer understanding of the condition, its risk factors, symptoms, diagnosis, potential complications, and treatment options. By staying informed and adhering to recommended guidelines, individuals can proactively manage their health and well-being.
For more comprehensive information and personalized guidance, consulting with a qualified healthcare professional is always advisable.
Tips for Managing Type II Diabetes Mellitus
To effectively manage Type II Diabetes Mellitus, individuals can incorporate the following practical tips into their daily routines:
Tip 1: Prioritize Regular Physical Activity
Engaging in regular physical activity enhances insulin sensitivity and improves glucose utilization. Aim for at least 150 minutes of moderate-intensity exercise or 75 minutes of vigorous-intensity exercise per week.
Tip 2: Maintain a Healthy Diet
Adopt a balanced diet rich in fruits, vegetables, and whole grains. Limit processed foods, sugary drinks, and unhealthy fats. Choose nutrient-dense foods that promote satiety and help regulate blood sugar levels.
Tip 3: Monitor Blood Sugar Levels Regularly
Regular blood sugar monitoring allows individuals to track their glucose levels and make necessary adjustments to their diet, exercise, and medication regimen. Consult with a healthcare professional to determine an appropriate monitoring schedule.
Tip 4: Adhere to Prescribed Medications
If prescribed medications are part of the treatment plan, it is crucial to adhere to the dosage and schedule as directed by the healthcare provider. Medications can effectively manage blood sugar levels and prevent complications.
Tip 5: Quit Smoking
Smoking negatively impacts blood sugar control and increases the risk of complications. Quitting smoking is essential for overall health and diabetes management.
Tip 6: Manage Stress
Chronic stress can elevate blood sugar levels. Engage in stress-reducing activities such as yoga, meditation, or spending time in nature to promote relaxation and well-being.
Tip 7: Get Enough Sleep
Adequate sleep is vital for overall health, including diabetes management. Aim for 7-9 hours of quality sleep each night to regulate hormones and improve insulin sensitivity.
Tip 8: Seek Support
Connect with support groups or consult with registered dietitians, certified diabetes care and education specialists, or other healthcare professionals for guidance, motivation, and emotional support.
By incorporating these tips into a holistic management plan, individuals with Type II Diabetes Mellitus can effectively control their blood sugar levels, reduce the risk of complications, and improve their overall health and well-being.
It is important to note that these tips are general recommendations, and individual needs may vary. Always consult with a qualified healthcare professional for personalized advice and guidance.
Conclusion
Type II Diabetes Mellitus is a complex chronic condition that requires ongoing management and lifestyle modifications. This article has explored the various aspects of Type II Diabetes Mellitus, including its causes, symptoms, diagnosis, treatment, prevention, and management.
Understanding these aspects is crucial for individuals to take an active role in managing their health and well-being. By adopting healthy lifestyle choices, adhering to treatment plans, and seeking support when needed, individuals can effectively control their blood sugar levels, reduce the risk of complications, and live fulfilling lives.
Youtube Video: