Pathophysiology of type 2 diabetes refers to the sequence of events at the cellular and molecular level that lead to the development and progression of type 2 diabetes, a chronic metabolic disorder characterized by elevated levels of blood glucose (sugar).
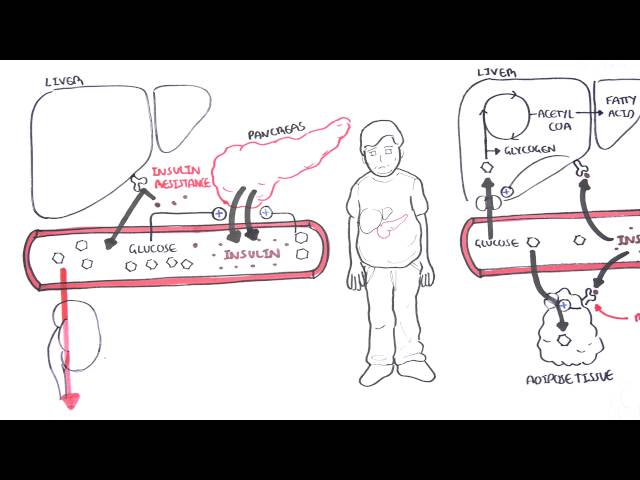
In type 2 diabetes, the body becomes resistant to the effects of insulin, a hormone produced by the pancreas that helps glucose enter cells for energy production. This insulin resistance leads to a buildup of glucose in the bloodstream, which can damage blood vessels and organs over time.
The exact cause of type 2 diabetes is unknown, but it is thought to be caused by a combination of genetic and environmental factors. Risk factors for type 2 diabetes include obesity, physical inactivity, a family history of diabetes, and certain ethnicities.
There is no cure for type 2 diabetes, but it can be managed with medication, diet, and exercise. Treatment aims to lower blood glucose levels and prevent complications.
Pathophysiology of Type 2 Diabetes
Understanding the pathophysiology of type 2 diabetes is crucial for developing effective prevention and treatment strategies. Key aspects to consider include:
- Insulin resistance: The body’s cells become less responsive to insulin, leading to a buildup of glucose in the blood.
- Beta-cell dysfunction: The pancreas produces less insulin, further contributing to elevated blood glucose levels.
- Increased glucose production: The liver produces more glucose, exacerbating hyperglycemia.
- Impaired insulin secretion: The pancreas releases insulin less effectively in response to glucose levels.
- Inflammation: Chronic inflammation is linked to insulin resistance and beta-cell dysfunction.
- Genetic factors: Certain genetic variations increase the risk of developing type 2 diabetes.
These key aspects are interconnected and contribute to the development and progression of type 2 diabetes. For instance, insulin resistance leads to increased glucose production and impaired insulin secretion, creating a vicious cycle that further elevates blood glucose levels. Understanding these mechanisms is essential for developing targeted therapies and lifestyle interventions to prevent and manage type 2 diabetes.
Insulin resistance
Insulin resistance is a key component of the pathophysiology of type 2 diabetes. Insulin is a hormone that helps glucose enter cells for energy production. When cells become resistant to insulin, glucose cannot enter as easily, leading to a buildup of glucose in the blood. This hyperglycemia, or high blood sugar, is a characteristic feature of type 2 diabetes.
Insulin resistance can be caused by a variety of factors, including obesity, physical inactivity, and certain genetic variations. When a person is obese, they have excess body fat that can release inflammatory chemicals into the bloodstream. These chemicals can damage cells and make them less responsive to insulin. Physical inactivity can also lead to insulin resistance, as muscles are one of the main tissues that take up glucose from the blood. Finally, certain genetic variations can increase the risk of developing insulin resistance.
Insulin resistance is a serious condition that can lead to a number of complications, including heart disease, stroke, kidney disease, and blindness. It is important to manage insulin resistance to prevent these complications. Lifestyle changes, such as losing weight, eating a healthy diet, and getting regular exercise, can help to improve insulin sensitivity. Medications may also be necessary to manage insulin resistance and type 2 diabetes.
Understanding the connection between insulin resistance and type 2 diabetes is crucial for developing effective prevention and treatment strategies. By targeting insulin resistance, we can help to prevent or delay the onset of type 2 diabetes and its associated complications.
Beta-cell dysfunction
Beta-cell dysfunction is a key component of the pathophysiology of type 2 diabetes. Beta-cells are cells in the pancreas that produce insulin, a hormone that helps glucose enter cells for energy production. When beta-cells become dysfunctional, they produce less insulin, leading to a buildup of glucose in the blood. This hyperglycemia, or high blood sugar, is a characteristic feature of type 2 diabetes.
- Reduced insulin production: Beta-cell dysfunction can lead to a decrease in insulin production. This can be caused by a variety of factors, including inflammation, oxidative stress, and genetic defects.
- Impaired insulin secretion: Even if beta-cells are producing insulin, they may not be able to secrete it properly. This can be caused by defects in the beta-cell’s secretory machinery.
- Increased beta-cell death: Beta-cells can die prematurely due to a variety of factors, including inflammation and oxidative stress. This can lead to a decrease in the number of beta-cells and a further reduction in insulin production.
Beta-cell dysfunction is a serious condition that can lead to a number of complications, including heart disease, stroke, kidney disease, and blindness. It is important to manage beta-cell dysfunction to prevent these complications. Lifestyle changes, such as losing weight, eating a healthy diet, and getting regular exercise, can help to improve beta-cell function. Medications may also be necessary to manage beta-cell dysfunction and type 2 diabetes.
Understanding the connection between beta-cell dysfunction and type 2 diabetes is crucial for developing effective prevention and treatment strategies. By targeting beta-cell dysfunction, we can help to prevent or delay the onset of type 2 diabetes and its associated complications.
Increased glucose production
Increased glucose production is a key component of the pathophysiology of type 2 diabetes. The liver is responsible for producing glucose through a process called gluconeogenesis. In healthy individuals, gluconeogenesis is tightly regulated to ensure that blood glucose levels remain within a normal range. However, in individuals with type 2 diabetes, gluconeogenesis is dysregulated, leading to excessive production of glucose.
There are several factors that can contribute to increased glucose production in type 2 diabetes, including:
- Insulin resistance: Insulin is a hormone that helps to suppress glucose production in the liver. In individuals with type 2 diabetes, insulin resistance leads to decreased suppression of glucose production.
- Increased glucagon levels: Glucagon is a hormone that stimulates glucose production in the liver. In individuals with type 2 diabetes, glucagon levels are often elevated, further contributing to increased glucose production.
- Defects in glucose sensing: The liver has specialized cells that sense glucose levels and adjust glucose production accordingly. In individuals with type 2 diabetes, these glucose-sensing mechanisms may be impaired, leading to increased glucose production even when blood glucose levels are already elevated.
Increased glucose production is a serious concern because it can lead to hyperglycemia, or high blood sugar. Hyperglycemia can damage blood vessels and organs over time, leading to complications such as heart disease, stroke, kidney disease, and blindness. Therefore, it is important to manage increased glucose production in individuals with type 2 diabetes to prevent these complications.
Lifestyle changes, such as losing weight, eating a healthy diet, and getting regular exercise, can help to improve glucose control and reduce glucose production. Medications may also be necessary to manage glucose production in individuals with type 2 diabetes.
Understanding the connection between increased glucose production and type 2 diabetes is crucial for developing effective prevention and treatment strategies. By targeting increased glucose production, we can help to prevent or delay the onset of type 2 diabetes and its associated complications.
Impaired insulin secretion
Impaired insulin secretion is a key component of the pathophysiology of type 2 diabetes. Insulin is a hormone that helps glucose enter cells for energy production. When the pancreas does not secrete insulin effectively in response to glucose levels, glucose builds up in the blood, leading to hyperglycemia, or high blood sugar.
- First-phase insulin secretion: The pancreas normally releases a burst of insulin in response to a rise in blood glucose levels. This first-phase insulin secretion is impaired in individuals with type 2 diabetes.
- Second-phase insulin secretion: The pancreas also releases insulin in a more sustained manner over time to keep blood glucose levels stable. This second-phase insulin secretion is also impaired in individuals with type 2 diabetes.
- Defects in insulin granules: Insulin is stored in the pancreas in vesicles called insulin granules. In individuals with type 2 diabetes, there may be defects in the insulin granules that impair insulin secretion.
- Islet amyloid polypeptide: Islet amyloid polypeptide (IAPP) is a hormone that is co-secreted with insulin. In individuals with type 2 diabetes, IAPP may form amyloid deposits in the pancreas, which can impair insulin secretion.
Impaired insulin secretion is a serious concern because it can lead to hyperglycemia, or high blood sugar. Hyperglycemia can damage blood vessels and organs over time, leading to complications such as heart disease, stroke, kidney disease, and blindness. Therefore, it is important to manage impaired insulin secretion in individuals with type 2 diabetes to prevent these complications.
Lifestyle changes, such as losing weight, eating a healthy diet, and getting regular exercise, can help to improve insulin secretion. Medications may also be necessary to manage impaired insulin secretion in individuals with type 2 diabetes.
Understanding the connection between impaired insulin secretion and type 2 diabetes is crucial for developing effective prevention and treatment strategies. By targeting impaired insulin secretion, we can help to prevent or delay the onset of type 2 diabetes and its associated complications.
Inflammation
Chronic inflammation is a key component of the pathophysiology of type 2 diabetes. Inflammation is a complex biological process that involves the activation of the immune system in response to injury or infection. In the context of type 2 diabetes, chronic inflammation can lead to insulin resistance and beta-cell dysfunction, both of which contribute to the development and progression of the disease.
- Adipose tissue inflammation: Adipose tissue, or body fat, is a major source of inflammation in individuals with type 2 diabetes. When adipose tissue becomes inflamed, it releases a variety of pro-inflammatory cytokines, which can damage cells and tissues throughout the body. These cytokines can also interfere with insulin signaling, leading to insulin resistance.
- Islet inflammation: The islets of Langerhans are clusters of cells in the pancreas that produce insulin. In individuals with type 2 diabetes, the islets can become inflamed, leading to damage and dysfunction of beta-cells. This can result in decreased insulin production and impaired insulin secretion, both of which contribute to hyperglycemia.
- Systemic inflammation: Chronic inflammation can also occur in other tissues and organs in the body, such as the liver, muscle, and blood vessels. This systemic inflammation can contribute to insulin resistance and beta-cell dysfunction, as well as the development of other complications of type 2 diabetes, such as cardiovascular disease and kidney disease.
Understanding the connection between inflammation and type 2 diabetes is crucial for developing effective prevention and treatment strategies. By targeting inflammation, we can help to prevent or delay the onset of type 2 diabetes and its associated complications.
Genetic factors
Genetic factors play a significant role in the pathophysiology of type 2 diabetes. Genome-wide association studies have identified over 100 genetic variants that are associated with an increased risk of developing type 2 diabetes. These genetic variants are thought to affect the function of genes that are involved in insulin signaling, glucose metabolism, and beta-cell function.
For example, one common genetic variant is associated with a decreased expression of the insulin receptor. This can lead to insulin resistance, which is a key factor in the development of type 2 diabetes. Another common genetic variant is associated with an increased production of glucose by the liver. This can lead to hyperglycemia, or high blood sugar, which is another characteristic feature of type 2 diabetes.
Understanding the genetic basis of type 2 diabetes is important for several reasons. First, it can help us to identify individuals who are at high risk of developing the disease. This can lead to earlier diagnosis and treatment, which can help to prevent or delay the development of complications. Second, understanding the genetic basis of type 2 diabetes can help us to develop new treatments for the disease. For example, researchers are currently developing drugs that target specific genetic variants that are associated with type 2 diabetes.
Frequently Asked Questions about the Pathophysiology of Type 2 Diabetes
Question 1: What is the pathophysiology of type 2 diabetes?
Answer: Type 2 diabetes is a chronic metabolic disorder characterized by elevated blood glucose levels due to insulin resistance, impaired insulin secretion, and increased glucose production. Insulin resistance occurs when cells become less responsive to insulin, leading to a buildup of glucose in the blood. Impaired insulin secretion results in decreased insulin production and impaired insulin release from the pancreas. Increased glucose production refers to the liver producing more glucose, further contributing to hyperglycemia.
Question 2: What are the risk factors for type 2 diabetes?
Answer: Risk factors for type 2 diabetes include obesity, physical inactivity, a family history of diabetes, certain ethnicities, and certain genetic variations.
Question 3: What are the symptoms of type 2 diabetes?
Answer: Symptoms of type 2 diabetes can include increased thirst, frequent urination, increased hunger, unexplained weight loss, fatigue, blurred vision, and slow-healing sores.
Question 4: How is type 2 diabetes diagnosed?
Answer: Type 2 diabetes is diagnosed through blood tests that measure blood glucose levels, such as the fasting plasma glucose test or the oral glucose tolerance test.
Question 5: How is type 2 diabetes treated?
Answer: Treatment for type 2 diabetes typically involves lifestyle changes, such as losing weight, eating a healthy diet, and getting regular exercise. Medications may also be necessary to lower blood glucose levels and improve insulin sensitivity.
Question 6: What are the complications of type 2 diabetes?
Answer: Complications of type 2 diabetes can include heart disease, stroke, kidney disease, blindness, and nerve damage.
Understanding the pathophysiology of type 2 diabetes is crucial for developing effective prevention and treatment strategies. By understanding the underlying mechanisms of the disease, we can work towards preventing its onset and managing it effectively.
Transition to the next article section:
For more information on the pathophysiology of type 2 diabetes, please refer to the following resources:
Tips for Understanding the Pathophysiology of Type 2 Diabetes
Understanding the pathophysiology of type 2 diabetes is crucial for developing effective prevention and treatment strategies. Here are a few tips to help you better grasp the complex mechanisms underlying this condition:
Tip 1: Focus on Key ConceptsStart by understanding the fundamental concepts of insulin resistance, impaired insulin secretion, and increased glucose production. These three factors are central to the pathophysiology of type 2 diabetes.Tip 2: Explore the Role of Adipose TissueAdipose tissue plays a significant role in type 2 diabetes. Its inflammation can lead to insulin resistance and contribute to the development of the disease.Tip 3: Examine Islet DysfunctionInvestigate the function of the islets of Langerhans in the pancreas and how their dysfunction can result in impaired insulin secretion, leading to hyperglycemia.Tip 4: Consider Genetic FactorsRecognize the influence of genetic variations on the risk of developing type 2 diabetes. Certain genetic variants can affect insulin signaling, glucose metabolism, and beta-cell function.Tip 5: Study Systemic InflammationComprehend the role of chronic inflammation throughout the body in the pathophysiology of type 2 diabetes. Systemic inflammation can contribute to insulin resistance and beta-cell dysfunction.Tip 6: Integrate Knowledge from Multiple SourcesUtilize various resources, including textbooks, scientific journals, and reputable websites, to gain a comprehensive understanding of the pathophysiology of type 2 diabetes.Tip 7: Seek Expert GuidanceConsult with healthcare professionals, such as doctors, nurses, or diabetes educators, to clarify complex concepts and obtain personalized advice.Tip 8: Stay Updated on ResearchKeep abreast of the latest research and advancements in the field to enhance your understanding of the pathophysiology of type 2 diabetes and its implications for prevention and treatment.By following these tips, you can develop a deeper understanding of the pathophysiology of type 2 diabetes, which is essential for effective management and prevention strategies.
Summary: Understanding the pathophysiology of type 2 diabetes is a critical step toward preventing and managing this condition. By focusing on key concepts, exploring the role of adipose tissue and islet dysfunction, considering genetic factors, studying systemic inflammation, integrating knowledge, seeking expert guidance, and staying updated on research, you can gain a comprehensive understanding of this complex disease.
Transition to the conclusion: With a solid understanding of the pathophysiology of type 2 diabetes, we can work towards developing more effective strategies to prevent its onset and manage it effectively.
Conclusion
The pathophysiology of type 2 diabetes is a complex and multifaceted process involving insulin resistance, impaired insulin secretion, and increased glucose production. Understanding these mechanisms is crucial for developing effective prevention and treatment strategies.
Research has shed light on the role of adipose tissue inflammation, islet dysfunction, genetic factors, and systemic inflammation in the development and progression of type 2 diabetes. By targeting these underlying factors, we can work towards preventing the onset of the disease and improving outcomes for those affected.
Further research is needed to fully elucidate the pathophysiology of type 2 diabetes and identify novel therapeutic approaches. However, the current understanding of the disease process provides a strong foundation for the development of comprehensive and effective management strategies.
Youtube Video: